Community of care
University-sponsored health clinics are common across the nation, but the Richmond Health and Wellness Program (RHWP) spearheaded by the VCU School of Nursing has earned a reputation as a model for holistic care coordination. Started in 2012, the program delivers weekly wellness clinics that focus on health assessment, monitoring, and coaching in five community-based sites across the Richmond region. Powered by about 100 VCU students guided by faculty each semester, RHWP offers education on effective chronic disease self-management , wellness coaching through healthy cooking demonstrations and diet management education, and care coordination to proactively manage other health issues and related social needs before they develop into emergencies. Last year alone, the program served 437 unique individuals over a total of 2,883 visits.
An interprofessional education model
In ten years the program has evolved, incorporating students from across VCU’s health science disciplines including nursing, pharmacy, medicine, social work, physical therapy, occupational therapy, health and kinesiology , and psychology. Participants can take part in clinic either with a scheduled 30-minute wellness visit or as a walk-in for unplanned or immediate needs. Kathie Falls, MSN, RN, ANP-BC, director of clinical operations for RHWP, explains that identifying gaps in care, supporting referrals, and promoting self-efficacy and self-management are key services that the program delivers. “RHWP is a safety net for our participants who are at high risk for negative health outcomes. Our healthcare system is complicated and can be hard to navigate when a person has limited access to transportation, technology, or low health literacy. We know that if we can connect people to services and necessary resources and provide tailored education, we can help people self-manage their healthcare needs and improve outcomes,” she says.
Visits frequently center around helping residents understand their conditions, how to proactively manage them and connecting them to information and resources. “By meeting people where they are and really listening to what’s important to them, we can tailor our services to their specific needs, which makes all the difference. We’re here to advocate for people and empower them to ask for what they need. When necessary, we can step in and help them articulate their needs to providers and health care workers whether in the emergency room or in their primary care provider’s office. We can help them tell their story,” Falls says.
Real life lessons
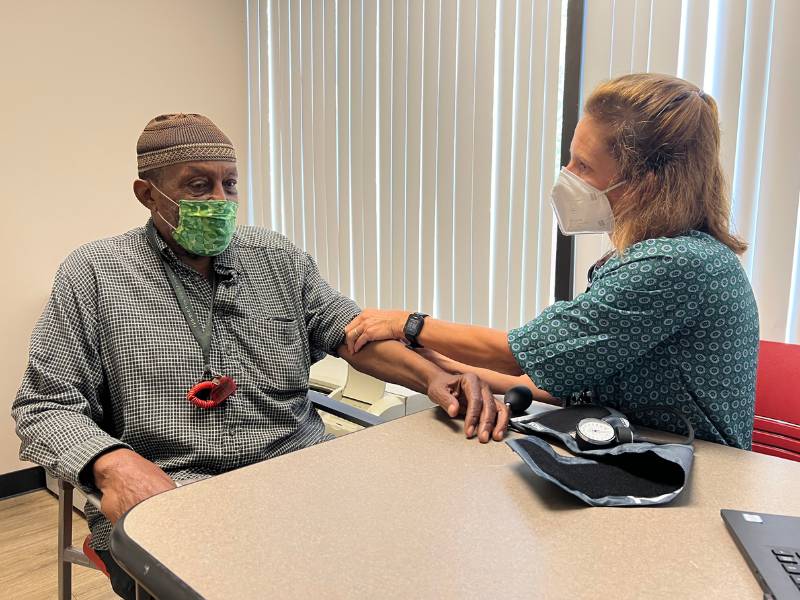
RHWP presents a range of opportunities for students to test out their future in collaborative health care. Clinic days start with a debrief from a program leader to touch on any immediate health concerns for any scheduled participants as well as general updates for the day. Then, students are given space to help participants independently, making notes on each visit using a shared secure data records platform with the program leader and staff available nearby for support. Students rotate through various positions during their time with the clinic. For example they might be assigned to assist with monitoring blood pressure or glucose one day, then provide more comprehensive self-management and education during the next visit. Following participant visits, program leaders and students reconvene to review notes and create a plan for the participant’s next visit.
Opportunities for students to integrate practice in a clinic setting like those that RHWP provides are invaluable. Kimberly Battle, Ph.D., FNP-BC, clinical assistant professor in the Department of Family and Community Health Nursing, describes the potential of the learning environment students experience in RHWP clinics and how it is integral to their understanding of health promotion and wellness implementation. “We have to realize with our students that everyone comes from different backgrounds. It’s important to teach students compassion, to teach them how to relate so that they can integrate into their own practice, how they think about affordability. Having [the student] ask ‘Is this realistic? This plan that I am developing for my participant that I’m interacting with?’” she explains. As Battle shares with those students in clinic that she supervises, the most instructive and influential lessons may come from an unexpected source. “We teach students how to listen to the participants and how they can learn from everyone,” she says.
Many students who start with RHWP to satisfy a service-learning requirement opt to continue their service. As a result, the School of Nursing is working to create an elective version of the course as well as a badge pathway so students can continue providing community service and receive either credit or recognition for their work as they move toward graduation and seek employment. The
deep engagement and strong rapport RHWP has with its participants is indicative of the quality of interactions with program leaders and students. “Social isolation is a huge issue for older adults in general, particularly older adults with limited income. The pandemic absolutely made this situation worse. At RHWP, we provide a forum for an intergenerational connection between our participants and the students who are able to listen to the concerns and needs of our participants and provide tailored education and feedback,” says Falls. “I see it all the time–our participants open up to students about things they’ve been afraid to ask in the past. Maybe they’re embarrassed or haven’t been able to find the words, but they ask the students and they get an answer."
New horizons
With a decade of success as its foundation, RHWP continues to grow. A recent grant of nearly $4 million in funding from the Health
Resources & Services Administration will enable the program to reach new communities with the addition of a mobile van. “We are taking our program on the road [...W]e have such a history with our program that we recognize that there are hot spots for chronic disease. We look forward to bringing a prescription produce program to these areas. We look forward to bringing our Richmond Health and Wellness interprofessional educational model. And, we look forward to bringing the nursing students to these areas where we can bring our education and care coordination and start to build trust and rapport in these areas and establish these relationships,” says Battle.
Visits by the numbers
Last academic year, clinics across five sites served 437 individuals in 2,883 visits. Over 1,400 students have participated since the program began. In fall of 2022, 122 students completed their clinical rotations with RHWP including 38 undergraduate nursing students, 38 nurse practitioner students, 38 pharmacy students, four medical students and four doctorate of physical therapy students.