Why VCU Nursing?

Be your best.
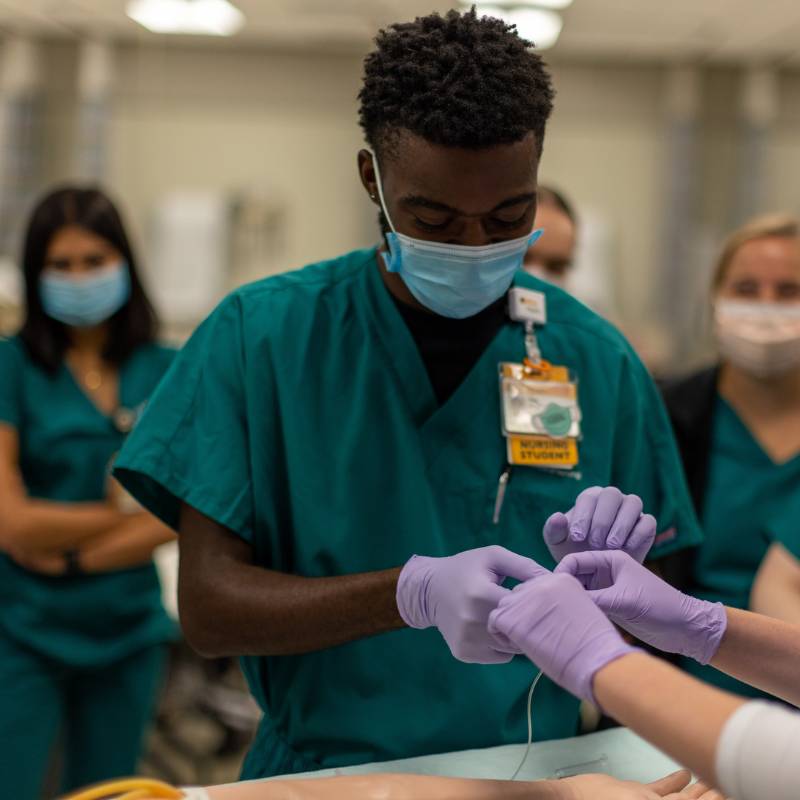
Earn your degree in a top program with the right support. From the moment you come through our doors, you are connected to a dedicated academic coaching and advising team, millions of dollars in annual scholarships and a learning environment that will help you be your best. You’ll learn from a diverse and experienced faculty who are excited to introduce you to the profession.
- Ranked in the top 5% of nursing B.S. programs in the nation in the latest U.S. News & World Report Best Colleges rankings
- $4 million+ awarded in annual scholarships
Our Academic Programs
News
April 16, 2024
Nursing oncology research award leads to NCI grant
April 9, 2024
Meet a researcher: Carla Nye, D.N.P.
Events
Nursing Spotlight

Ready to be a RAM?
Your future is UNLIMITED.